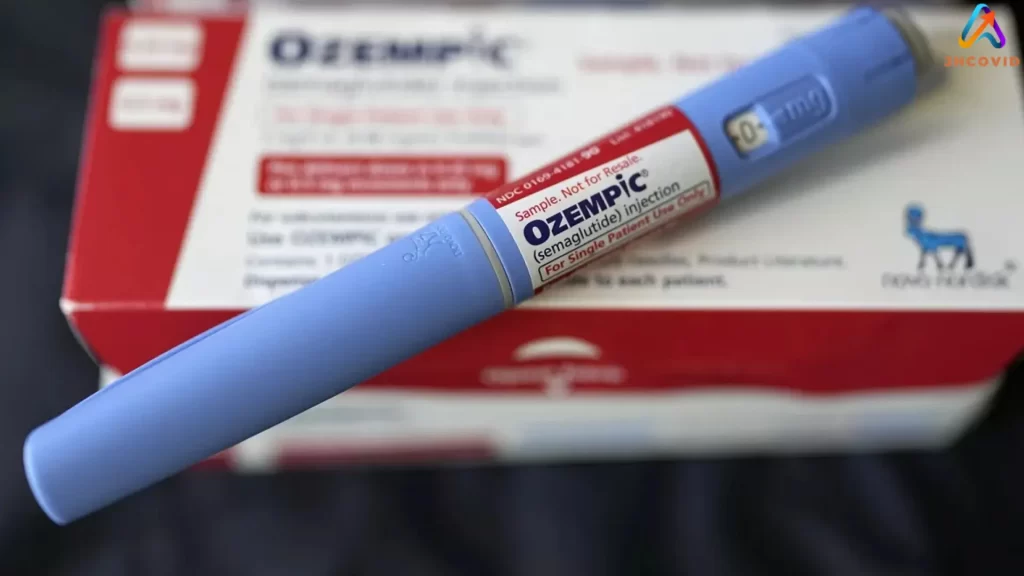
In recent months, the use of Ozempic and Wegovy has drawn attention not just for their weight loss benefits but also for the troubling rise in cases of gastroparesis among users. Gastroparesis, a condition characterized by delayed stomach emptying, has been reported more frequently in patients using these GLP-1 agonists.
This alarming trend raises questions about the safety and long-term effects of these medications, which were initially celebrated for their effectiveness in managing diabetes and obesity.
Patients have experienced severe nausea, vomiting, and even cases of stomach paralysis, highlighting the urgent need for healthcare providers to monitor and address these adverse effects. Although many users see an improvement in gastroparesis symptoms after discontinuing the medication, some report persistent issues that linger for months.
These ongoing symptoms and the current status of the Ozempic class action lawsuit have significant implications for both patients and pharmaceutical companies.
The connection between Ozempic, Wegovy, and gastroparesis underscores the importance of informed medical guidance and patient awareness, especially when considering the dose of semaglutide, such as 1 mg injections. By recognizing the potential risks associated with semaglutide and engaging in open conversations with healthcare providers, patients can better navigate their treatment options and avoid severe complications.
Understanding Gastroparesis and Its Connection with Diabetes
Gastroparesis, a condition characterized by delayed gastric emptying, is significantly linked to diabetes and can be a common side effect of Ozempic. This section delves into the pathophysiology of gastroparesis, the impact of GLP-1 analogs in diabetes management, and the incidence and awareness of gastroparesis, particularly among diabetic patients.
The Pathophysiology of Gastroparesis
Gastroparesis is often a result of damage to the vagus nerve, which controls the movement of food in the digestive tract, and can be exacerbated by using Ozempic injections. In diabetic patients, high blood sugar levels can cause nerve damage, making it essential to consult a healthcare provider about the effect of Ozempic.
This leads to stomach paralysis, where the stomach muscles cannot function properly, causing severe nausea and other gastrointestinal issues.
Delayed gastric emptying prevents the stomach from emptying food normally, further complicating blood sugar control, a known side effect of Ozempic.
Role of GLP-1 Analogues in Managing Diabetes
GLP-1 agonists, such as semaglutide (marketed as Ozempic, Wegovy, and Rybelsus), effectively manage type 2 diabetes in adults by enhancing insulin secretion and slowing gastric emptying. These medications also aid in weight loss, which is beneficial for diabetic management, particularly for those who take Ozempic.
However, they have been known to experience various side effects, including those related to Ozempic. Linked to gastroparesis in some patients, the side effects of Ozempic may be more pronounced.
Gastroparesis is an adverse event associated with these medications, characterized by symptoms like nausea, vomiting, and stomach paralysis, which may occur when patients take Ozempic.
Incidence and Awareness of Gastroparesis
Gastroparesis is more common in patients with diabetes, affecting approximately one-third of these individuals, particularly those who use Ozempic. The cumulative incidence over ten years is higher in those with type 1 diabetes compared to type 2 diabetes, especially among those using Ozempic.
Despite its impact, gastroparesis remains a relatively rare and under-recognized complication of diabetes, particularly among those using semaglutide. Increasing awareness among patients and healthcare providers is crucial for early diagnosis and effective management of this condition, especially using GLP-1 agonists for diabetes treatment.
Notably, recent studies have highlighted that the rate of gastroparesis is about 10 cases per 1,000 semaglutide users who take Ozempic, indicating a potential side effect of Ozempic.
Exploring Treatment Options and Potential Side Effects

Treatment options for managing gastroparesis, particularly related to medications like Ozempic, include a mix of drugs, diet modifications, and lifestyle changes that can help improve symptoms. It’s crucial to understand the potential side effects of medications like Ozempic and weigh them against the benefits of these treatments.
Weight Management Strategies in Diabetic Patients
Managing weight in diabetic patients often involves using GLP-1 receptor agonists like Ozempic, Saxenda, and Victoza. These drugs promote weight loss by reducing appetite and slowing gastric emptying, which can benefit blood sugar management.
Diet and Exercise: Maintaining a healthy lifestyle is essential for adults with type 2 diabetes. Diet control, including smaller, more frequent meals and a balanced nutritional intake, improves weight management and helps regulate blood sugar levels. Exercise also plays a vital role in enhancing insulin sensitivity and aiding weight loss, which can be beneficial for those using Ozempic.
Medication: Discussing the appropriate dose of drugs like Ozempic with healthcare providers is essential. Medications such as metformin or off-label options like bupropion-naltrexone are used in combination with lifestyle changes to improve outcomes, especially for patients using Ozempic.
Doctors may also consider the use of newer drugs like tirzepatide, which show promise in weight reduction for adults with type 2 diabetes.
Assessing the Risks of GLP-1-Related Medications
GLP-1 related medications like Ozempic are effective but come with risks. Nausea and vomiting are common side effects. Other gastrointestinal issues include diarrhea, constipation, and abdominal pain.
Severe Complications: Rarely, do patients experience delayed gastric emptying leading to conditions like gastroparesis. Biliary disease and acute gallbladder disease are also reported.
Monitoring and Treatment Adjustments: Regular monitoring by a gastroenterologist or endocrinologist is essential. Adjusting dosages or switching medications might be necessary if severe side effects occur.
Alternatives and Adjunctive Therapies
When GLP-1 medications are unsuitable, other treatments and adjunct therapies are considered.
Alternative Medications: Bupropion-naltrexone or drugs like Saxenda offer different mechanisms for weight control.
Diet and Lifestyle Adjustments: Emphasizing a meticulously controlled diet and regular physical activity can be highly effective. Surgery, such as gastric bypass, might be an option for managing severe obesity resistance to other treatments.
Supportive Therapies: Patients might benefit from off-label uses of certain medications to manage symptoms and improve gastric motility. Consulting with specialists ensures a tailored approach to each patient’s needs.
Also Read: Att Data Breach 2024 Lawsuit Compensation: Can You Get Paid?
Final Thought
It is evident that the use of Ozempic and Wegovy is associated with cases of gastroparesis. This condition can cause significant discomfort, affecting patients’ quality of life.
Gastroparesis manifests through symptoms such as severe nausea, vomiting, bloating, and early satiety. Studies indicate that semaglutide users experience gastroparesis at a rate of about 10 cases per 1,000 users.
This condition’s delayed gastric emptying is particularly challenging. For instance, delayed gastric emptying impacts food digestion significantly, often leading to prolonged periods of discomfort and unpredictability in nutrient absorption.
Management of semaglutide-induced gastroparesis includes monitoring symptoms and adjusting medication as needed. Clinicians play a crucial role in ensuring patient tolerability, emphasizing the importance of individualized treatment plans.
The awareness around these adverse effects is growing. It is crucial to weigh the benefits of Ozempic and Wegovy against the risks, especially for patients with pre-existing gastrointestinal issues.
The potential for these treatments to cause significant symptoms calls for careful consideration. Patients and healthcare providers should maintain open communication to promptly address any concerning symptoms.
Understanding the ramifications of these medications enables more informed decisions in diabetes and obesity management. This knowledge is essential for developing effective and safe treatment plans.
Addressing gastroparesis requires a collaborative approach. By staying informed and vigilant, patients and healthcare providers can better manage these side effects. Enhanced education and awareness about the risks associated with these medications can lead to improved patient outcomes.






